
–by Dr. Peng E. Wang
Introduction
The phrase “pink eye” describes the inflammation of the outer transparent layer of the eye, also known as conjunctivitis (Wiki). Although the condition is most commonly due to a viral infection, there are other non-infectious cases of conjunctivitis. Pink eye is a common experience for most of us at least once in our lifetime. Understanding the cause of conjunctivitis helps to understand the optimization of its management. While the symptoms of different types of pink eye are similar, some differences should be considered. For instance, should you stay home if you have pink eye? What causes the pink eye to occur? How long is it contagious? Will it go away without treatment? In this article, we will discuss the symptoms and management of conjunctivitis.
Overview
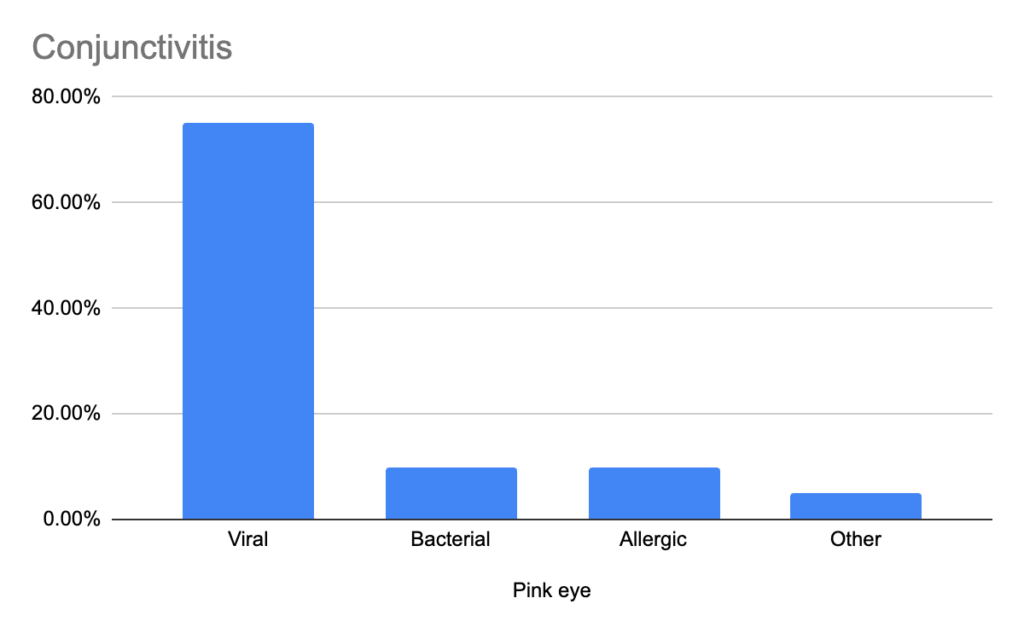
Most of the cases of pink eye are caused by viral infections (NCBI). Bacterial conjunctivitis is less common, and allergies also affect the eyes. Autoimmune disorders such as Sjogren’s disease and rheumatoid arthritis can affect the eyes as well, although much less common. In general, it’s difficult to determine the cause of conjunctivitis during the early stages, but understanding patterns can offer guidance to quarantine and reduce transmission of infections.
Associated symptoms offer hints of what may be causing the pink eye, and the timeline of its progression also entails a guide to the next steps in management.
The management of pink eye shares commonalities, but also some differences based on complications, duration of the symptoms, and associated symptoms. The best self-diagnostic questions to ask are
- Did you come in contact with ill persons? You can get pink eye from the same virus when others do not.
- How long has it been? More than three days? Consider medical evaluation.
- Visual changes that are persistent? Please seek urgent medical attention.
- Fever, sore throat, cough, or congestion? Likely viral.
- Are the eyelids affected? Yes? Likely bacterial.
- Mostly itching without mucus? Likely allergies.
- Are there any other associated cold symptoms? Likely viral.
- Wearing contacts? Yes? They can cause dry eyes and corneal abrasions (NCBI).
Viral conjunctivitis
Seldom are the symptoms limited to just the eyes, and 90% of cases are due to adenovirus; only 1.3% – 4.8% are due to herpes virus (NCBI); considering >95% of the population carries different strains of the herpes virus.
- Diffuse redness of white parts of the eyes
- Eyes itching
- Light sensitivity
- Discharge clear
- Tearing excessively
- Lymph node swelling just in front of the ear and under the chin
- Typically affects both eyes but starts with one eye
- Commonly associated with cold symptoms (fatigue, aches)
If you are experiencing cold-like symptoms in addition to pin eye, avoid contact with others and wash your hands frequently to reduce transmission. The infectious period of conjunctivitis lasts 10-14 days (NCBI). It’s impractical to be quarantined for a prolonged period, so practice contact precautions. Viral conjunctivitis resolves on its own, but treatments can help facilitate it.
Related article: The Common Cold Symptoms and Treatments
Bacterial conjunctivitis
- Diffuse redness of white parts of the eyes
- Eye pain with the feeling of swelling
- Eye foreign body feeling (grittiness)
- Sticky, yellowish discharge
- Crusting of eyes and surrounding area
- Eyelid swelling and redness, dryness, crusting
- Eyelids get stuck together, especially the mornings
- More localized symptoms in the ear, nose, throat, and eyes
Similar symptoms resemble a viral pink eye but with some differences. The most common bacteria that cause conjunctivitis in children are Haemophilus and Staphylococcus in adults (NCBI). Bacterial pathogens cause more localized symptoms compared to viral pathogens, so it’s not associated with generalized symptoms such as fatigue and body aches. While it’s not practical to quarantine for pink eye, contact precautions are warranted, so practice good hygiene. Typically, bacterial conjunctivitis should be treated with antibiotic eye drops.
Allergic conjunctivitis
Allergies-induced pink eye symptoms are typically not associated with any fever, aches, chills, etc.
- The start of the symptoms typically involves BOTH eyes
- Itching and redness underneath the eyelids (bulbar/palpebra)
- Swelling of the conjunctiva (edema)
- Minimal crusting in the mornings
- Tearing and mucus production
- Purplish discoloration of eyelids
- Swelling around eyes
The history and presentation of allergic conjunctivitis are distinctly different than infectious conjunctivitis, especially if the symptoms are seasonal, come and go, and are prolonged. Although there are distinct symptoms of allergic conjunctivitis versus viral and bacterial pink eye, the early stages are still difficult to tell the difference.
Other causes of conjunctivitis
Foreign body induced (common)
- Corneal abrasion due to eye injuries or use of contact lenses
Autoimmune (NCBI)
- Rheumatoid arthritis
- Crohn’s disease
- Celiac disease
- Psoriasis
- Sjogren’s disease
- Myasthenia gravis
- Grave’s disease
- Hashimoto’s thyroiditis
- Systemic sclerosis
Exposure (AAO)
| Acidic | Alkali |
| Bleach | cleaning agents |
| Batteries | fertilizers |
| Refrigerant | drain cleaners |
| Glass polishing agent | firework sparklers, flares |
| Vinegar | plastar, mortar, cement |
| Swimming pools | caustic potash |
This is not a comprehensive list of pink eye causes, and it’s difficult to separate between conjunctivitis and other associated eye disorders, such as keratoconjunctivitis sicca, scleritis, keratitis, blepharitis, uveitis, etc.
Conjunctivitis Treatments
Recommended
Supportive management
- Warm compresses to help break up thickened oil that congests the eyelids
- Cool compresses for swelling and pain
- Light avoidance and reduced screentime to reduce eye strain
- Stop using contact lenses until the issue has been resolved
- Eye lubricants
Lubricants (over-the-counter)
- Refresh Gel Tears, the active ingredient is carboxymethylcellulose, artificial tears only
- TheraTears Dry Eye, active ingredient is carboxymethylcellulose, artificial tears only
Why do we recommend lubricants in the case of pink eye since excessive mucus is already occurring? Because the mucus being made is pro-inflammatory and is not in pH balance. You want to reduce the inflammatory mucus and replace it with natural tears to soothe the eyes.
Allergies eye drops (over-the-counter)
- Optivar, the active ingredient is azelastine, helps with conjunctivitis related to allergies
- Zaditor, the active ingredient is ketotifen
- Alaway, the active ingredient is ketotifen
- Pataday, the active ingredient is Olopatadine
- Zyrtec Itchy Eye Drops
- Similasan Hay Fever, natural antihistamine Euphrasia with sterile neutral pH
Antibiotics (prescription only)
- Erythromycin is the active ingredient for this eyedrop, great for eyelid-involved pink eye
- Tobrex, the active ingredient is tobramycin, eye drops for viral and bacterial pink eye
- Ciloxan, the active ingredient is ciprofloxacin, used if you are allergic to erythromycin
Do not recommend
Eye decongestants
- Naphcon, the active ingredient is naphazoline, can increase eye (ocular) pressure (IOP)
- All Clear, the active ingredient is naphazoline
- Clear Eyes, the active ingredient is naphazoline
- Visine Advanced Relief
- Visine Redness Relief
Eye steroids (risk of increased ocular pressure)
- Durezol, the active ingredient is difluprednate
- Lotemax, the active ingredient is ioteprednold
- Many more variants exist, and they all require a prescription
Complications and prevention
When to see a doctor (urgent)
- Ptosis, eyelid swelling that can obstruct vision
- Persistent visual disturbance or vision loss
- Eye issues fail to improve after 5 days
- Nausea with severe eye pain (increased eye pressure)
- Notable ulceration or foreign body appears on conjunctiva
- Corneal lesion or ulceration (the clear dome of the eye)
- Corneal blood (blood in the clear part of your eyeball)
While acute conjunctivitis has rare complications, they can occur, particularly if you are not certain of the diagnosis of pink eye. Herpes conjunctivitis has the highest risk of complications, up to 38.2% (NCBI), thus if you have shingles or herpes simplex and it’s affecting your eye, seek urgent care to reduce the risk of vision loss.
Prevention
- Good hygiene especially hand washing
- PPE (person protective equipment) use such as goggles
- Hydrate your eyes when they feel dry with artificial tears
- Avoid using decongestant eye drops
- Avoid using contact lenses past their recommended time
- Monitor your screen time and adjust your screen accordingly
- Mac OS has “Night Shift” to reduce blue light
- Windows OS has “Nightlight” to reduce blue light
- Wear blue light glasses with or without a prescription for extended screen time
Your eyes are your “window” to your life, so protect them with the most caution to avoid serious life-altering injuries.
Conclusion:
While it is impossible to cover all potential reasons for “pink eye” in this article, there are trends helpful to know for its management. If your symptoms are consistent with viral origins, which is the most common, consider quarantine if your work and lifestyle allow it (remote work). Practicing universal contact precautions is crucial to reduce transmission if work and life events are unavoidable. When complications occur after the onset of pink eye, you should seek medical attention. Many treatments are available for conjunctivitis, including supportive management, natural products, and pharmaceuticals, but it’s also important to know what to avoid. In case of prolonged eye symptoms, consider the less common or rare conditions, which will require a comprehensive workup.
Bonus: Antibiotic Eye Drops
Can antibiotic eye drops help in cases of conjunctivitis? The short answer is yes. Antibiotics typically are non-selective, meaning they reduce all microbes. While it’s not generally recommended for the common cold since it’s difficult to tell the difference between viral and bacterial, the argument here is that the result at the tissue level is the same: inflammation. See antibiotics as an indirect anti-inflammatory. Reducing the microbial burden on inflamed tissue reduces symptoms and transmission. This argument is sound for topical antibiotics only, not systemic (oral) antibiotics. Since antibiotics are non-selective, they will reduce the good microbes in your airway, gastrointestinal tract, and urinary system when taken orally; this puts you at risk for other infections.

Related article: The Common Cold Symptoms and Treatments