–by Dr. Peng E. Wang
Introduction
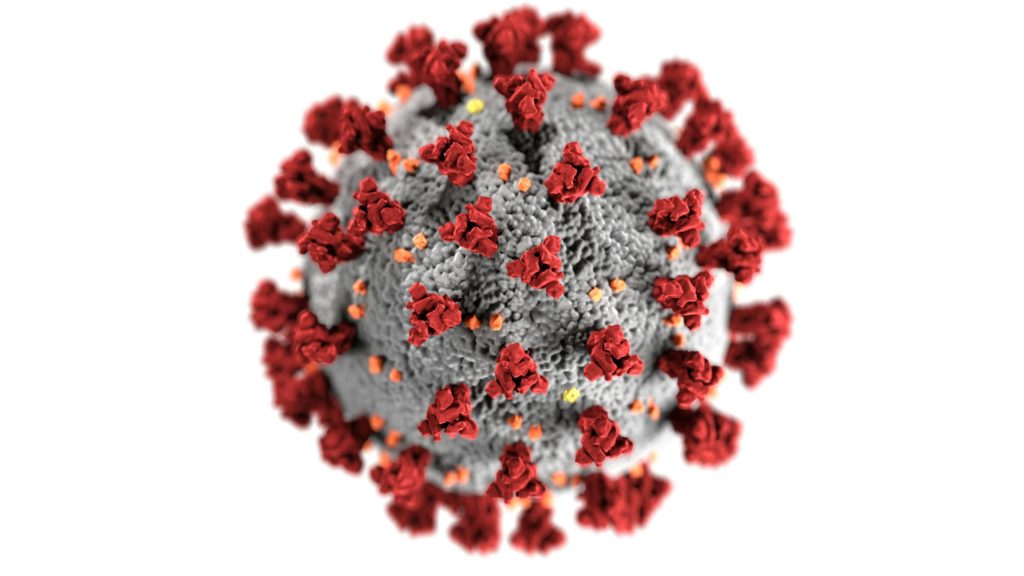
Coronavirus is in a class of its own. SARS and MERS-related outbreaks occurred before COVID-19 (Wiki), and these coronaviruses caused epidemics without a pandemic, unlike COVID-19 (SARS-CoV-2). In the United States, the first reports of a coronavirus were in the 1920s on chicken called Infectious Bronchitis Virus (IBV), and human cases were discovered by the Common Cold Unit in Great Britain in the 1960s. The new class of virus was finally categorized as the “corona” virus after their appearance under the microscope resembled a sphere with spikes. Understanding coronavirus history offers guidance and pattern recognition of severe respiratory illnesses. In this article, we compare COVID-19 today vs. in 2020 and discuss the management of symptoms to prevent complications.
| COVID-19 in 2020 | COVID-19 in 2023 |
| Alpha, beta | Omicron (BA, JN.1) predominant |
| Aggressive respiratory illnesses | Upper respiratory infections (colds) |
| Severe cough, loss of smell | Cough, congestion, sore throat |
| Fever >101F persistent | Fever <100F or none |
| pneumonia, bronchitis | sinusitis, bronchitis |
| Nausea, diarrhea | Severe diarrhea (JN.1) |
| Less infectious, more fatal | More infectious, less fatal |
| Incubation 5 days | Incubation 3 days |
| Mortality rate ~6% (NCBI) | Mortality rate <3% (NCBI) |
Overview
The novel COVID-19 coronavirus in 2019 into 2020 was very aggressive, and the mortality rate was significant due to complications (NCBI). So, what are the current symptoms of COVID-19 in 2023? In general, it’s less severe, and it’s more representative of a common cold. The beginning of COVID-19 in 2023 may feel like a cold, starting with headaches, sore throat, runny nose, fatigue, and sneezing (Wiki). The symptom of the new COVID going around is diarrhea, in addition to respiratory symptoms, and the new Omicron variant is JN.1 at the time of this writing (JH). With a sudden onset of cold-like symptoms, it’s no longer safe to assume it’s a cold, so you should consider testing for COVID-19 to minimize transmission. Overall, the new COVID variants are more infectious and have faster onset but shorter symptom duration.
Many organisms can cause upper respiratory symptoms, and there are patterns you should recognize to suspect COVID. Management for COVID and the common cold is similar but has some distinct differences. The main difference is the risks of complications due to systemic effects, especially in the elderly and young people with chronic health issues.
It’s important to know what not to do when you have COVID-19; many treatments are available for an upper respiratory infection, and some remedies can worsen the progression of the illness, so it’s important to know what remedies to use and avoid.
The COVID-19 Symptoms in 2023
Symptoms of COVID occur an average of 3.5 days (NCBI), and the symptoms last between 4 (vaccinated) to 7 days (Wiki).
Common
- Runny nose
- Cough
- Congestion
- Headache
- Fatigue
- Sore throat
- Sneezing
Less common
- Fever >100.4 °Fahrenheit (38 °Celsius)
- Loss of smell (anosmia)
- Diarrhea (JN.1) is becoming more common
Rare symptoms (Seek immediate care)
- Palpitations or fast heart rate due to dehydration
- Lightheaded and nearly passing out (presyncope)
- Chest pain
- Shortness of breath
Early recognition of COVID-19 symptoms can help you decide when to isolate. Additionally, it provides an estimate of the quarantine period and monitoring of the symptom progression. More importantly, the rare symptoms call for immediate evaluation because “walk-in” pneumonia can occur as complications. Pneumonia means there is a fluid collection in your lower airway, and bronchitis means you have a fluid collection in your mid-airway; these phrases do not equal bacterial infection.
COVID-19 Treatments
Recommended
Self-care tips
- Drink fluids with electrolytes (Gatorade, Smart Water, etc.)
- Dress in layers of clothing so you can adjust as needed
- Sleeping propped up about 30 degrees to reduce drainage
- Monitor your oxygen level (goal > 90%) by purchasing a pulse oximeter
- Monitor your heart rate level (goal < 120) by purchasing a pulse oximeter
- Supplements including Zinc and multivitamins can increase the co-factors your body needs to fight the infection since they will be utilized more
- Natural remedies such as honey, Echinacea, Elderberry, and Eucalyptus reduce the toxicity/irritability of the mucus thus helping with painful throat and reducing inflammation in turn
Antihistamines type 1; over-the-counter; best to be scheduled
- Claritin, the active ingredient is loratadine, with fast onset in one hour if taken on an empty stomach
- Clarinex, active ingredient is desloratadine, an analog of Claritin, has fewer side effects
- Zyrtec, active ingredient is cetirizine, with fast onset in one hour if taken on an empty stomach
- Xyzal, the active ingredient is levocetirizine, an analog of Zyrtec, with fewer side effects
Antihistamines type 2; over-the-counter; reduces nausea by reducing acid
- Pepcid, the active ingredient is famotidine, has a fast onset in 1 hour, lasts 10 hours, and can be taken with food
Fever and pain reducer; over-the-counter
- Tylenol, active ingredient is acetaminophen, 500mg or 325mg, use as needed
Nasal steroid topicals; over-the-counter; as needed
- Flonase, the active ingredient is fluticasone propionate, slow onset, alcohol-based solution
- Nasacort, the active ingredient is mometasone, slow onset, non-alcohol based solution (less likely to cause nosebleed)
Cough suppressants; over-the-counter; as needed
Cough suppressants; Prescription; as needed
- Tessalon Perles, the active ingredient is Benzonatate, prescribed for common colds, and persistent cough
- Codeine is a common narcotic that functions through the mu receptor pathway (controlled prescription)
Non-steroid Anti-inflammatory Drugs (NSAID); best to be scheduled
**Avoid if you have nausea, indigestion, or diarrhea, use Tylenol instead
Multisymptoms cold remedy (only one recommended)
- Nyquil, active ingredients are acetaminophen, doxylamine, and dextromethorphan; as needed only
Reactive cough > 10 days use Inhaled corticosteroids; prescription only; best to be scheduled
- Fluticasone, known as Flovent, the powder form was discontinued; aerosol (HFA) available
- Mometasone, known as Asthmanex; aerosol (HFA) and Twisthaler (powder)
- Budesonide, known as Pulmicort; aerosol (HFA) or nebulized only
- Advair Diskus, fluticasone/salmeterol; with a long-acting form of albuterol, twice daily
- AirDuo Respiclick, fluticasone/salmeterol; same as Advair but has a generic, less expensive, twice-daily
- Breo Ellipta, fluticasone/vilanterol; only once daily, expensive
- Symbicort HFA, budesonide/formoterol, aerosol only
- Wixela, fluticasone/salmeterol; same as Advair, but has generic, less expensive, twice daily
Do Not recommend
Over-the-counter cold remedies (Ironically)
- Dayquil, active ingredients include phenylephrine and guaifenesin
- Nyquil Sinus, active ingredients include phenylephrine
- Alka-Seltzer Plus Severe Allergy Sinus Congestion & Headache
- Mucinex Cold/Flu, active ingredients include phenylephrine, a decongestant
- Any packaging that states “Cold and Sinus” and “Cold and Flu”
Mucus relief (expectorants)
- Mucinex, the active ingredient is guaifenesin, also in Robitussin and many cold medicines
- Mucinex Children’s Stuffy Nose
- Mucinex Sinus-Max Clear & Cool
Decongestants (Hides well in many remedies, look at the ingredients)
- Afrin nasal spray, the active ingredient is oxymetazoline
- QlearQuil 12-Hour Nasal Decongestant Moisturizing Spray
- Vicks Sinex 12-Hour
- Vicks Sinex Severe Decongest
- Mucinex Children’s Stuffy Nose
- Mucinex Sinus-Max Clear & Cool
- Dayquil, active ingredients include phenylephrine
Behind the counter
- Claritin-D, active ingredients are loratadine and pseudoephedrine
- Zyrtec-D, active ingredients are cetirizine and pseudoephedrine
- Allegra-D, active ingredients are fexofenadine and pseudoephedrine
- Mucinex-D, active ingredients are guaifenesin and pseudoephedrine
Antibiotics
- Z-pack, active ingredient is azithromycin
It depends…
- Paxlovid, the active ingredients are nirmatrelvir and ritonavir; reduces viral replication and must be within 120 hours of symptoms onset.
Paxlovid side effects include changes in taste (dysgeusia) and diarrhea, which are mild. However, these medications remain controversial, especially if your symptoms are mild cold-like symptoms. If you are taking other medications, they can interfere with Paxlovid. Due to these factors, you should meet certain criteria (HHS) before considering it, so it should not be an automatic recommendation.
Complications and Prevention
When you have COVID, the initial response of your body’s immune response is hyperactivity with mucus production and dilation of the arteries inside your airway. This occurs in the local region involving your sinuses, nasal cavity, and glands (tonsils); removing tonsils early isn’t a great idea since it’s a part of your immune system (Wiki).
Physical defense system against pathogens (NCBI)
- Nasal hairs block pathogens from entering
- Mucus trapping pathogens (mucus has its purpose)
- The angle between the pharynx (throat) and your nasal cavity prevents falling of pathogens into the airway
- Tonsils are your first immune response to a pathogen
- Ciliated hairs move mucus upward only keeping pathogens away from the lungs
Your body is trying to quarantine pathogens with mucus and inflammation while preventing mucus from accumulating in the lower airways (lungs). It is crucial to understand what not to do to increase the challenge. Ultimately, the challenge in a respiratory infection is to overcome impaired oxygen delivery due to fluid accumulation. Cold remedies with decongestants and expectorants risk fluid buildup in your airway and risk these complications.
Complications (post-infection)
- Middle ear infection; ear pains and fever >100.4F
- Serous otitis media; fluid behind the eardrum and hearing loss
- Bronchitis; fluid in the mid-airway causing wheezing, shortness of breath, and fever
- Pneumonia; fluid in the lower airway causing fever, fatigue, shortness of breath, and very ill feeling
When to see a doctor (non-emergent)
- Fever recurring after the initial fever has resolved
- Ear pain with a fever
- Sinus impaction (not draining) with a fever
- Cough lasting > 10 days without shortness of breath
Prevention
*Vaccination- regardless of how you feel about vaccines, this article is not debating the politics of it, but the science of it is that it reduces complications. While the COVID-19 vaccines do not eliminate infections, they should make it milder and reduce the risk of complications and hospitalizations (NCBI).
- Avoidance of contact with ill individuals
- PPE (personal protective equipment) including masks and glasses
- Hand washing after contact
- Disinfect fomites (physical objects that were in contact with ill persons)
- Adequate sleep, exercise, and hydration
- Vitamin D3 to boost vitamin D levels (NIH)
Conclusion
When comparing COVID-19 now and in 2020, the symptoms are overall less severe and commonly represent common cold symptoms. Antivirals have side effects, and interactions with other medications are a common concern. With the onset of cold or flu-like symptoms, there are things you should be doing and not doing to optimize the symptoms control. A sound management plan should reduce excessive drainage and exaggerated inflammatory response while avoiding complications. Many medications do the opposite, namely Mucinex and Dayquil. Your body’s defense system tries to quarantine and destroy the pathogens while learning and ready for the next time. With many treatment options available for COVID, it’s best to prevent and minimize complications, so get vaccinated, get adequate sleep, exercise, eat a healthy diet, and boost your vitamin D level since most of us are deficient.
Bonus: Decongestants, why you should avoid it
Can decongestants make you drain more and increase the risk of pneumonia? Possibly. The mechanism is more open airway by compressing the arteries lining the airway, thus allowing more space for drainage and more stomach upsets. Decongestants also cause rebound congestion, with elevated heart rate and blood pressure to a dangerous level. The difference between a vein and an artery is the amount of smooth muscle they are made of. Arteries have three layers of smooth muscle, and veins only have one. Veins are more elastic and compliant. Arteries are not very compressible. If you forcibly squeeze arteries by using decongestants, rebound congestion ensues. Bottles of nasal decongestants, such as Afrin (oxymetazoline), and others like phenylephrine in cold remedies, it’s best to avoid it.

Related article: The Cold Symptoms and Treatments