
–by Dr. Peng E. Wang
Introduction
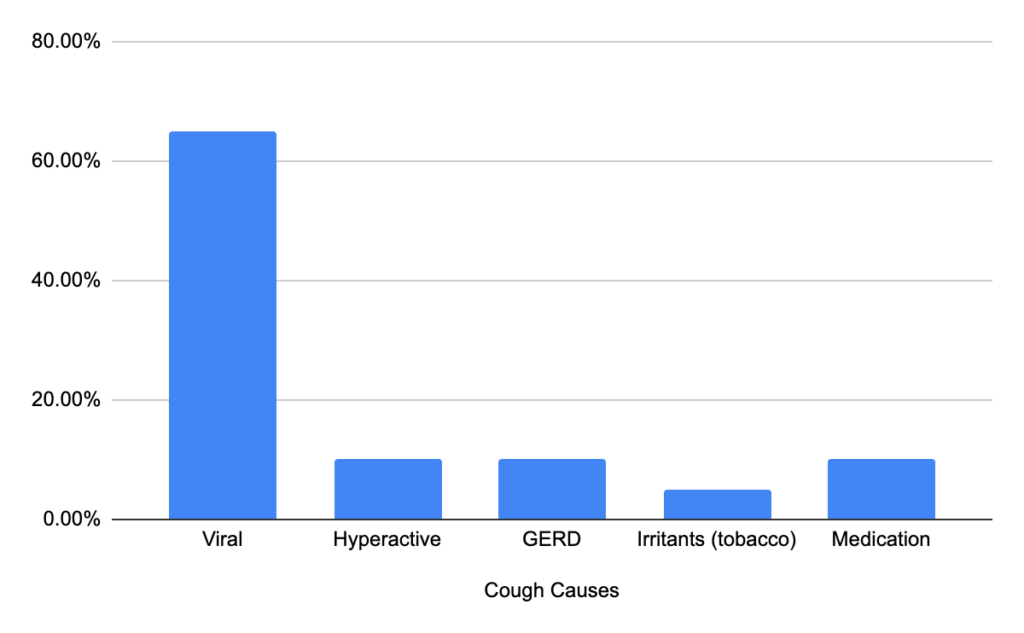
Cough is considered a protective reflex (Wiki). There are many reasons for a cough, such as a viral infection inducing the cough reflex in the host (you) to help spread itself for the continued gain of survival. Not all coughs are due to an infection; others include medications (i.e. Lisinopril), reactive and hyperactive airway (allergic), sinus drainage, and acid reflux. When you have a cough, it’s crucial to determine the cause of the cough rather than solely focusing on the treatments. You are likely aware that all medications can cause side effects; more is not necessarily better.
1. Viral infection
If you Google “upper respiratory infection”, there are hundreds of possible causes, which is overwhelming. What is the exact cause of my cough? And what are the diagnostics and treatments available? All valid questions, but while pondering for a potential workup, are there things you can do to facilitate the management? Absolutely; by answering a few questions.
- Less than 3 days and not yet done an in-home COVID test? Consider in-home COVID test.
- Came in contact with young children? They are the perfect vectors for viruses, even without any symptoms.
- Less than 2 weeks and improving? More time is needed.
- More than 2 weeks and not going away? Time to chat with a healthcare provider.
- Is mucus coming up? Taking a mucus reliever (i.e. guaifenesin, Mucinex)?
- Have you tried stopping the mucus reliever that may be making it worse?
- Throat irritation, dry/tickling cough and not going away? Tried using an antihistamine (i.e. Zyrtec) to reduce the drainage?
- Had fever/aches/fatigue? No? It may not be viral but due to other causes.
- Had fever initially, then resolved, but fever is back after > 1 week? It’s time to chat with a healthcare professional.
- Used mucus relief, decongestants, and cold remedies. Tried to stop the meds first?
- Chest tightness, wheezing, or shortness of breath? Time to seek immediate care.
You should know that viruses do not directly induce a cough; they do so via immune pathways (reactive). There are numerous other pathogens in the environment, likely more than 3 billion estimated, and there are over 5 million fungal (mold) species alone. Your airway becomes more reactive or hyperactive to the surrounding pathogens after a viral infection, and drainage with a cough occurs. Regardless of the molecular (immunological) reasons, at the tissue level, it involves histamines, inflammation, swelling, and mucus production.
2. Hyperactive airway
Allergies can cause a cough via postnasal drainage. Similar to hyperactive airway disease like asthma, it can cause a cough. If you think about it, asthma and allergies are “hyperactive” diseases all cause airway swelling due to smooth muscle hypertrophy (engorgement). The airway system, including your sinuses, is lined with mucosal cells and thus is called mucosal membrane. Allergens induce mucous cells in your airway system to make mucus via inflammatory pathways, commonly induced by immune triggers involving histamine release. If you have a history of seasonal or perennial (year-round) allergies and a cough, you should ask yourself a few questions about the onset of a cough.
- Fever? Yes? Unlikely to be allergies.
- Throat irritation or scratchy throat? Likely getting drainage.
- Recent seasonal change?
- Traveled and potentially exposed to new allergens?
- Got a new pet?
- Worked outdoors?
- Worked in a moldy basement?
- Tried antihistamines (i.e. loratadine, cetrizine, levocetirzine, desoloratadine)?
- Tried antihistamines but still have drainage. Did it on an empty stomach? No? You should.
- Tried nasal spray (i.e. fluticasone) but still getting drainage and cough.
- Used the nasal spray via the optimal technique?
- No drainage, but constantly coughing around certain times of the year?
- Tested for asthma?
- Tried an inhaler such as albuterol (no-steroid)?
- Flovent (steroid)?
3. Sinus drainage
Sinus drainage could be due to various reasons, including viruses, mold, and temperature changes (vasomotor). Try to avoid thinking of the term “sinusitis” as a singular and isolated disorder; it’s not. Commonly you hear the phrase sinusitis, which is the result of other causes; it is not synonymous with “infection”, either. Like everything in life, it’s how we perceive it. If you think sinusitis means infection, you aim for one treatment, antibiotics, which alone suboptimally address sinusitis and increase your risks of other illnesses. Sinusitis means sinus inflammation. When physicians try to code a diagnosis for sinus issues in your chart, there is no such diagnosis as “sinus infection” but only sinusitis. Similar to cough from allergies and drainage, ask yourself a few questions to facilitate the management of sinusitis.
- Fever and no indigestion/diarrhea? Viral cold-induced sinusitis cough.
- No fever, but having reflux and indigestion? Yes, GERD can cause sinusitis and cough.
- Have a history of GERD? On a daily PPI (i.e. omeprazole) to see if the cough stops?
- No fever, but seasonal changes and history of allergies? Likely allergic rhinitis –> sinusitis.
- Tried antihistamines (i.e. loratadine, cetrizine, levocetirzine, desoloratadine)? Twice a day?
- Tried antihistamines but still have drainage. Did it on an empty stomach? No? You should.
- Tried nasal spray (i.e. fluticasone)?
- Used the nasal spray via the optimal technique?
- Having pressure around your eyes?
- Tried NSAID (i.e. naproxen, ibuprofen)?
- Was NSAID scheduled? No? You should do 2 times daily with food only for ~3 days as a trial.
- Took scheduled antihistamines on an empty stomach with scheduled NSAID with food? No? Try it for ~3 days.
- >2 weeks with a feverish feeling or >99F? And you cannot expel any discharge? Time to seek professional care.
4. Acid Reflux
Did you know that acid reflux does not automatically mean heartburn? Even without heartburn/indigestion symptoms, a cough could be due to a gastrointestinal issue. Silent acid reflux can manifest as a cough, sore throat, and the feeling of something in the back of your throat constantly (Globus sensation). A significant amount of the U.S. population has GERD (gastroesophageal reflux disease) per the American College of Gastroenterology, which encompasses both heartburn and acid reflux symptoms. So if you have a lingering cough lasting >2 weeks, without fever or asthma history, you should be asking the following questions.
- Am I eating too late? Within 2 hours of bedtime
- Did I drink coffee within 4 hours of bedtime?
- Did I drink alcohol within 4 hours of bedtime?
- I did not do any of the above, do I have GERD?
- Am I snoring a lot at night?
- Do I wake up with a sore throat a lot?
- Do I wake up feeling there is something in my throat?
- Am I clearing my throat all the time?
- Have I tried Pepcid (famotidine) to see if my cough stops?
- Have I tried Prilosec (omeprazole) to see if my cough stops?
5. Medications
ACE inhibitors like Lisinopril, or any other generic medication name ending with -pril, can cause a cough in many users (Medscape). Medications such as Lisinopril inhibit ACE (angiotensin-converting enzyme), which is needed to hydrolyze bradykinin (Wiki). Bradykinin is a chemical that induces a cough reflex; recall that cough is a protective reflex. Your body needs a signal to expel contents from your airway when they are not desired, like fumes and pollutants. ACE breaks down bradykinin to reduce the cough reflex, and Lisinopril inhibits ACE. Lisinopril decreases the enzyme that reduces our cough reflex; double negative means positive, thus more cough. If all else is failing and you still have a lingering cough while taking prescription medications, talk to your doctor about alternatives. Some common medications that can induce a cough include
- Lisinopril, Enalapril, Captopril, Benazepril (bradykinin)
- Losartan (bradykinin), is four times less likely than Lisinopril to induce cough
- Sitagliptin (Januvia), worsens allergies
- Calcium channel blockers (i.e. Cardizem, diltiazem), acid reflux cough
- Beta Blockers (i.e. Metoprolol, Coreg), airway hyperactivity
- NSAID (i.e. ibuprofen), airway constriction by increasing asthma symptoms
Conclusion:
While it is impossible to cover all potential reasons for a cough in this article, these are common. Looking at the first three causes, they have the same reason ultimately, which involves sinus drainage. Your airway needs lubrication, commonly done by the baseline drippage from the sinuses. When invading pathogens or pollutants induces inflammatory drainage that irritates your airway, it makes you cough. Not to forget that acid reflux, or GERD, can make you cough via irritation of your upper airway from acid. If you have not tried lifestyle modifications, do that before grabbing an antacid from a pharmacy. Lastly, if all else fails and you are taking routine medications, it may be due to a medication, even if it’s the same medication you have been taking for years; you can develop side effects with any medicine at any one point.
Bonus: Decongestants, why you should not use it
Can decongestants make you cough more due to reflux? Yes. The mechanism is more open airway by compressing the arteries lining the airway, thus allowing more space for drainage and more stomach upsets. Decongestants also cause rebound congestion, with elevated heart rate and blood pressure to a dangerous level. The difference between a vein and an artery is the amount of smooth muscle they are made of. Arteries have three layers of smooth muscle, and veins only have one. Veins are more elastic and compliant. Arteries are not very compressible. If you forcibly squeeze arteries by using decongestants, rebound congestion ensues. Bottles of nasal decongestants, such as Afrin (oxymetazoline), and others like phenylephrine in cold remedies, it’s best to avoid it.

Related article: 7 Common Medications for Cough